Abstract
Background: Complete Blood Count (CBC) analytical capacity is falling short of recognizing informative RBC morphology or WBC dysplastic morphological changes. Current morphologic peripheral blood smear (PBS) analysis is performed manually using a semi-quantitative scale on a limited number of cells introducing high degree of subjectivity and low sensitivity. The novel Full-Field Morphology (FFM) technology developed by Scopio Labs performs PBS analysis on a significantly larger scale of 1000 fields of 100X view in a routine manner, allowing a precise and highly sensitive automated quantification of cellular and sub-cellular morphological parameters. Current diagnosis of myelodysplastic syndrome (MDS) is based on invasive bone marrow aspirate, followed by subjective morphological analysis. In this study, we applied this digital morphometric approach to compare PBS morphology of MDS patients with age-matched controls.
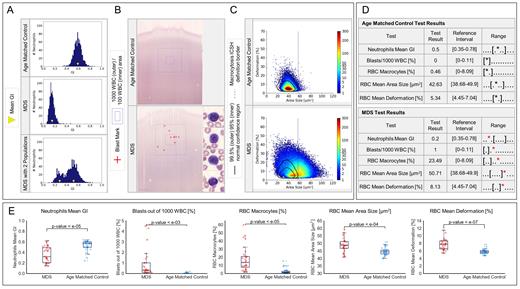
Methods: 32 MDS (average age 80+10, [range 41-97] y, F:M ratio 14:18) and 30 age-matched control (average age 79+9, [range 65-100] y, F:M ratio 13:17) PBS were scanned by the Scopio Labs system, and evaluated according to three distinct morphological features with known significance in MDS: blast percentage per 100 or 1000 WBC; neutrophil cytoplasmic granulation per 1000 neutrophils; RBC morphology of at least 150,000 RBC. Quantitative determination of neutrophils granulation, was measured by Granulation Index (GI, between 0-1) and GI Distribution Width (GIDW, between 0-1). RBC measurements included the quantitative measurements of RBC size, namely macro- and microcytosis, and RBC contour changes (deformation), i.e. the percent of RBC that deviate from normal RBC shape.
Results: The mean GI of MDS samples was 0.36+0.15, [range 0.14-0.63] (Fig. 1A middle, Fig. 1E), significantly (p<10 -4) lower compared with the mean GI of age-matched control samples 0.53+0.10, [range 0.24-0.64] (Fig. 1A top, Fig. 1E). Mean GI were highly diverse among MDS samples compared with age-matched controls (Fig. 1E), but with no significant differences in GIDW (not shown). Interestingly, two sub-populations of neutrophils were detected in some of the MDS samples, differ in their mean GI (0.26 for one sub-population, 0.52 for the second one, Fig. 1A bottom). Such fingerprint, suggesting the presence of an abnormal and normal clones, was not detected in the control samples. Percentage of blasts was determined per 100 or 1000 WBC counts/sample (Fig. 1B). Blasts were detected in 13/32 (41%) of MDS samples compared with 1/30 (3%) of age-matched controls, when counts were performed per 100 WBC. However, when 1000 WBC were analysed, blasts were detected in 27/32 (84%) of MDS samples compared with 6/30 (20%) of age matched controls, a highly significant difference (p<10 -6). The percentage of blasts per 1000 WBC counts/sample of MDS samples was 0.92+1.35, [range 0-5] %, significantly (P<0.0008) higher compared with the percentage of blasts per 1000 WBC counts/sample of age-matched control samples 0.02+0.05, [range 0-0.2] % (Fig. 1E). RBC analysis revealed significant differences between MDS and age-matched samples (Fig. 1C). As expected, mean RBC size (49+4, [range 41-59] mm 2 MDS; 45+3, [range 40-51] mm 2 age matched) and % of macrocytosis (17+15, [range 2-60] % MDS; 3+4, [range 0-15] % age matched) were significantly (p<10 -5) higher in the MDS samples compared with the age matched controls (Fig. 1E). We found that MDS PBS contained significantly (p<10 -6) higher number of abnormally-shaped RBC (8+1, [range 5-12] %), compared with age-matched controls (6+1, [range 5-8] %) (Fig. 1E). Representative summaries of morphometric analyses of MDS and age-matched control are shown in figure 1D. Representative PBS scans of MDS and control samples are available in https://demo.scopiolabs.com/?_org=VCdaE756rjYwZW3Z#/scans.
Conclusion:
Our study demonstrates that FFM-based digital PBS analysis enables the detection and quantification of unique WBC and RBC morphologic alterations associated with MDS. The expanding therapeutic options for MDS, including for patients at early disease stages, makes the establishment of an accurate diagnosis of MDS, even at early stages, to be highly important. The proposed novel digital imaging technology opens the opportunity to screen patients, diagnose them early, based on peripheral blood morphology, and potentially, monitor their responsiveness to therapy.
Katz: Scopio Labs: Consultancy. Karni: Scopio Labs: Current Employment. Shimoni: Scopio Labs: Current Employment. Natan: Scopio Labs: Current Employment. Shaham: Scopio Labs: Current Employment. Pozdnyakova: Scopio Labs: Consultancy. Mittelman: Janssen · Roche · Novartis · Takeda · Medison / Amgen · Neopharm / Celgene / BMS · Abbvie · Gilead: Research Funding; Novartis · Takeda · Fibrogen · Celgene / BMS · Onconova · Geron: Other: Clini; Onconova · Novartis · Takeda · Silence: Membership on an entity's Board of Directors or advisory committees; MDS HUB: Consultancy; Celgene / BMS · Novartis: Speakers Bureau. Avivi: Novartis: Speakers Bureau; Kite, a Gilead Company: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal